Pelvic Uterine Prolapse
da Vinci® Sacrocolpopexy Brochure
What is Pelvic Uterus Prolapse
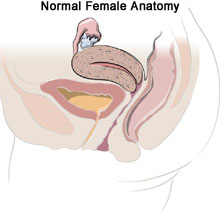
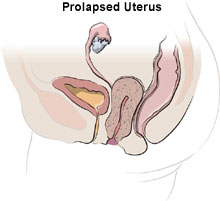
Pelvic Uterus Prolapse occurs when the pelvic muscles that support the uterus such as pelvic muscles, ligaments and other tissues weaken and sags. If the uterus drops out of its normal position, this is called prolapse. Prolapse is defined as a condition where organs slip or fall down toward the vagina and can sometimes cause a noticeable bulge. Our women’s health services include uterine prolapse treatment.
Vaginal Vault Prolapse
Pelvic prolapse is usually accompanied by some degree of vaginal vault prolapse. Vaginal vault prolapse occurs when the upper part of the vagina loses its shape and sags into the vaginal canal or outside the vagina. Pelvic prolapse may also involve sagging or slipping of other pelvic organs, including the bladder, the urethra and rectum.
Anatomy of the Vaginal Vault
Vaginal vault prolapse occurs when the upper part of the vagina sags or drops down. It is said to be located in the “ceiling” or the inner, upper end of the vagina. The vaginal vault has four “compartments”: an anterior compartment, closest to the front of the body; the vaginal wall; a middle compartment consisting of the cervix; and a posterior compartment consisting of the vaginal wall at the back of the body.
Signs & Symptoms of Pelvic Prolapse
Women with mild cases of pelvic prolapse may not experience noticeable symptoms. However, as the uterus falls further down, it can place pressure on other pelvic organs
Pelvic Prolapse Symptoms Include:
- Low back pain
- Sensation of sitting on a small ball
- Stretching or pulling in the pelvis
- Pelvic or abdominal pain
- Pain during intercourse
- Protrusion of tissue from the opening of the vagina
- Repeated bladder infections
- Spotting or Vaginal bleeding or an unusual or excessive discharge
- Problems with Bowel movements (Constipation)
- Frequent urination
Symptoms may become worse with standing or walking for long periods due to added pressure placed on the pelvic muscles.
Causes and Risk Factors1
Pelvic prolapse is usually caused by damage to the tissues that support the pelvic organs. Conditions that may contribute the cause of pelvic prolapse are, natural/vaginal births, low estrogen after menopause, Chronic coughing, heavy lifting and obesity.
Pelvic Prolapse Screening & Diagnosis
In order to Diagnose Pelvic Prolapse, your gynecologist must perform a pelvic examination. You will be asked about your medical history and symptoms. The examination will check for signs of prolapse.
Pelvic Prolapse Exams may include a:
- Ultrasound
- Magnetic resonance imaging (MRI)
- Cystoscopy
- Computed Tomography Scan (CT scan)
- Bladder function test
- Cotton swab test
- Pelvic floor strength test
Pelvic Prolapse Treatment
Women with mild uterine prolapse may not need treatment if they are not experiencing any symptoms. However, the pelvic floor may continue to loosen and cause the prolapse to become more severe. It is important to schedule checkups with your doctor to track the severity of the prolapse. In order to strengthen the pelvic muscles it is recommended to perform kegels, maintain a healthy weight, avoid heavy lifting, and treat other contributing medical problems.
Other Treatment options for more Severe Cases Include:
- Vaginal pessary
- Surgery
PN 1002244 Rev B 01/2014
- Uterine Prolapse; A service of the U.S. National Library of Medicine – National Institutes of Health. Available from: http://www.nlm.nih.gov/medlineplus/ency/article/001508.htm
Serious complications may occur in any surgery, including da Vinci® Surgery, up to and including death. Examples of serious or life-threatening complications, which may require prolonged and/or unexpected hospitalization and/or reoperation, include but are not limited to, one or more of the following: injury to tissues/organs, bleeding, infection and internal scarring that can cause long-lasting dysfunction/pain. Risks of surgery also include the potential for equipment failure and/or human error. Individual surgical results may vary.
Risks specific to minimally invasive surgery, including da Vinci Surgery, include but are not limited to, one or more of the following: temporary pain/nerve injury associated with positioning; temporary pain/discomfort from the use of air or gas in the procedure; a longer operation and time under anesthesia and conversion to another surgical technique. If your doctor needs to convert the surgery to another surgical technique, this could result in a longer operative time, additional time under anesthesia, additional or larger incisions and/or increased complications.
Patients who are not candidates for non-robotic minimally invasive surgery are also not candidates for da VinciSurgery. Patients should talk to their doctor to decide if da Vinci Surgery is right for them. Patients and doctors should review all available information on non-surgical and surgical options in order to make an informed decision. For Important Safety Information, including surgical risks, indications, and considerations and contraindications for use, please also refer to www.davincisurgery.com/safety and www.intuitivesurgical.com/safety. Unless otherwise noted, all people depicted are models.




